Dietary restraint and food addiction
By David A. Wiss & A. Janet Tomiyama
Food addiction cases should always be conceptualized in a psychosocial context, including life history and current mental health status. It is critical to assist individuals seeking a nutrition overhaul based on a food addiction diagnosis to have adequate resources, including the ability (and time) to prepare their own food and find a community of like-minded individuals on a similar path (i.e., social support). Inappropriate, excessive, or unsuccessful restraint can worsen a person’s quality of life. Inconsistent dietary restraint in which
periods of successful restriction are followed by loss-of-control eating is likely to exacerbate food addiction symptoms and increase eating disorder risk.
Subscribe for weekly insights and research exploring the link between nutrition & mental health.
Abstract
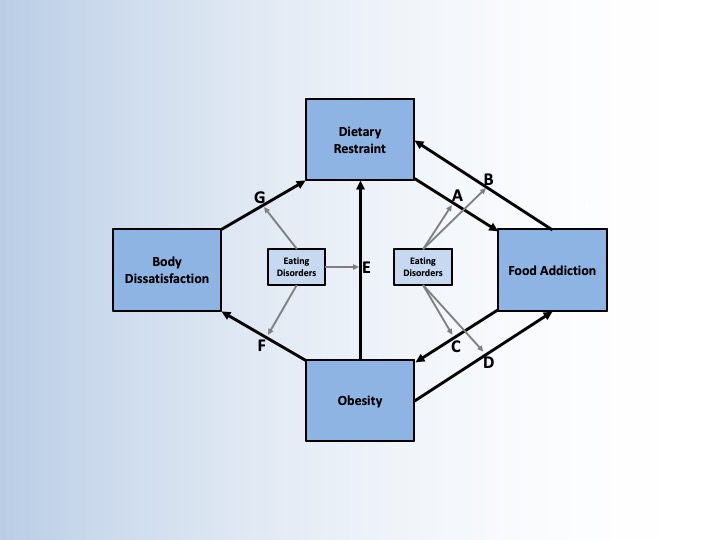
The goal of this chapter is to describe the interconnections between dietary restraint and food addiction. While vulnerability to food addiction through dietary restraint has not been established, there is merit in carefully examining the bidirectional connections between the two.
Our conceptual model highlights important additional connections between obesity and body dissatisfaction, as well as moderating roles of various eating disorders. Two clinical vignettes illustrate intricacies among these relationships, highlighting important and exciting future directions.
Recommendations for case conceptualization for professionals working with eating disorders and food addiction include consideration of the temporal sequence of symptom onset, the presence of comorbidities, and individualized treatment, which can discern as well as combine divergent food philosophies. Misguided treatments may lead to clinically significant eating disorders or worsen food addiction symptoms over the long run. A nuanced examination of the bidirectional relationship between dietary restraint and food addiction is timely and warranted.