Low carbohydrate and psychoeducational programs show promise for the treatment of ultra-processed food addiction
By Jen Unwin, Christine Delon, Heidi Giaever, Clarissa Kennedy, Molly Painschab, Frida Sandin, Charlotte Schön Poulsen, & David A. Wiss
The current data are the first to demonstrate the short-term clinical effectiveness of a low-carbohydrate “real food” intervention delivered in an online group format with education and social support for individuals with FA symptoms. Larger, controlled and randomized intervention studies are urgently needed to continue to explore ways to help people with this serious and multi-faceted condition which often goes undiagnosed and untreated. It would be extremely useful to compare this approach to more inclusive “all foods fit” approaches among those with co-occurring FA and EDs, particularly BED.
Subscribe for weekly insights and research exploring the link between nutrition & mental health.
Abstract
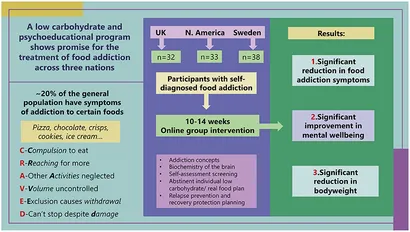
Food addiction, specifically ultra-processed food addiction, has been discussed in thousands of peer-reviewed publications. Although 20% of adults meet criteria for this condition, food addiction is not a recognized clinical diagnosis, leading to a dearth of tested treatment protocols and published outcome data.
Growing numbers of clinicians are offering services to individuals on the basis that the food addiction construct has clinical utility. This audit reports on clinical teams across three locations offering a common approach to programs delivered online. Each team focused on a whole food low-carbohydrate approach along with delivering educational materials and psychosocial support relating to food addiction recovery.
The programs involved weekly sessions for 10–14 weeks, followed by monthly support. The data comprised pre- and post- program outcomes relating to food addiction symptoms measured by the modified Yale Food Addiction Scale 2.0, ICD-10 symptoms of food related substance use disorder (CRAVED), mental wellbeing as measured by the short version of the Warwick Edinburgh Mental Wellbeing Scale, and body weight. Sample size across programs was 103 participants.
Food addiction symptoms were significantly reduced across settings; mYFAS2 score −1.52 (95% CI: −2.22, −0.81), CRAVED score −1.53 (95% CI: −1.93, −1.13) and body weight was reduced −2.34 kg (95% CI: −4.02, −0.66). Mental wellbeing showed significant improvements across all settings; short version Warwick Edinburgh Mental Wellbeing Scale 2.37 (95% CI: 1.55, 3.19). Follow-up data will be published in due course. Further research is needed to evaluate and compare long-term interventions for this complex and increasingly burdensome biopsychosocial condition.